Treatments
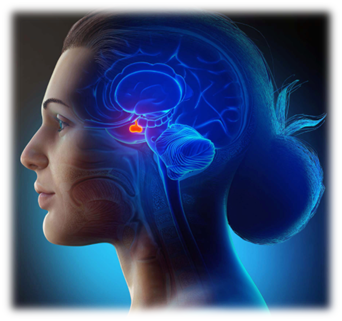
Endoscopic Surgery for Pituitary Adenoma
Pituitary Adenomas Most pituitary adenomas are non-cancerous tumours in the pituitary gland that don't spread bey
Pituitary Adenomas Most pituitary adenomas are non-cancerous tumours in the pituitary gland that don't spread bey