Endoscopic Surgery for Pituitary Adenoma
Pituitary Adenomas
Most pituitary adenomas are non-cancerous tumours in the pituitary gland that don't spread beyond the skull.
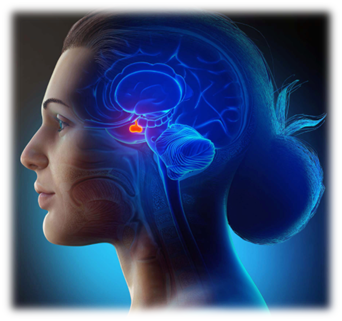
What is the pituitary?
Pituitary (hypophysis) is a pea-sized endocrine gland at the base of our brain, behind the bridge of your nose and directly below the hypothalamus. It sits in a cavity in the sphenoid bone called the sella turcica.
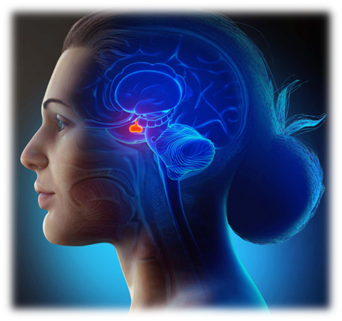
The pituitary is often referred to as the “master gland” because it not only secretes its own hormones, it sends commands to other glands to produce hormones.
What is a pituitary adenoma?
Pituitary adenomas are benign or non-cancerous tumors of pituitary gland, which means they remain localized and do not spread to other parts of the body .Most of them arise from anterior lobe of the gland.
How common are pituitary adenomas?
More than 1 million cases of pituitary adenomas are reported in India every year. Epidemiologic studies show that pituitary adenomas are increasing in incidence (between 3.9 and 7.4 cases per 100,000 per year) and prevalence (76 to 116 cases per 100,000 population) in the general population (approximately 1 case per 1000 of the general population).
What causes pituitary adenomas?
Scientists don’t know exactly what causes most pituitary tumors.
Some people inherit gene mutations (changes) from their parents that greatly increase their risk for developing pituitary tumors. But often, gene mutations occur during life rather than having been inherited. Most pituitary tumors are not cancers, and there are no known environmental causes for these tumors. The gene changes in these tumors might just be random events that sometimes happen when a cell divides, without having an outside cause.
Because there are no known lifestyle-related or environmental causes of pituitary tumors, it’s important to remember that there is nothing people with these tumors could have done to prevent them.
What are the symptoms of a pituitary adenoma?
A pituitary tumor causes symptoms in 3 different ways :
- By producing too much of 1 or more hormones:
- Growth hormone. The symptoms depend on a patient’s age. In children, before the bone plates have closed, increased growth can cause gigantism, which is excessive body size and height. In adults, increased growth hormone causes acromegaly, a syndrome that includes excessive growth of soft tissues and bones, high blood sugar, high blood pressure, heart disease, sleep apnea, increased snoring, carpal tunnel syndrome, and pain, including headaches.
- Thyroid stimulating hormone (TSH). Too much TSH causes increased production of thyroid hormone. This can lead to nervousness and irritability, fast heart rate and high blood pressure, heart disease, increased sweating, thin skin, and weight loss.
- Prolactin. Too much prolactin, a hormone that stimulates lactation and the secretion of progesterone, causes unexpected secretion of breast milk. It can also cause osteoporosis, which is weakening of the bones; loss of sex drive; infertility; irregular menstrual cycles; and the inability to have an erection.
- Adrenocorticotropic hormone (ACTH). Too much of this hormone causes weight gain, particularly in the body’s torso or trunk. It can also cause high blood pressure, high blood sugar, brittle bones, emotional changes, stretch marks on the skin, and easy bruising.
- Gonadotropins (FSH and LH). These are usually not high enough to cause symptoms but can, in rare cases, cause infertility and irregular menstrual cycles.
- By pressing on the pituitary gland, causing it to make too little of 1 or more hormones.
- Growth hormone. Not enough growth hormone causes late growth in children, poor muscle strength, irritability, weakening of bone strength, and an overall unwell feeling.
- TSH. Low TSH causes fatigue, low energy, sensitivity to cold temperatures, constipation, and weight gain.
- Prolactin. Too little prolactin causes an inability to breastfeed.
- ACTH. Too little of this hormone causes fatigue and low energy, low blood pressure, low blood sugar, and upset stomach.
- Gonadotropins. Low levels of gonadotropins cause infertility, decrease in sex drive, an inability to have an erection, and irregular menstrual cycles.
- As the pituitary adenomas grow in size, they may compress nearby structures.By pressing on the optic nerves or, less commonly, the nerves controlling eye movements, it can cause either loss of part or all of a person’s sight, or double vision.Large pituitary adenomas (pituitary macroadenomas) can also crush the normal pituitary cells and alter their regulatory activities.
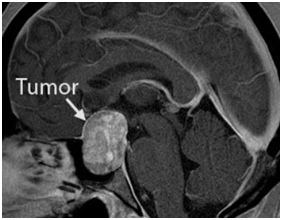
Microadenoma and Macroadenoma
Microadenomas are pituitary adenomas that measure less than 10 mm in diameter (about three quarters of an inch). A pituitary adenoma greater than or equal to 10 mm in diameter is called a macroadenoma.
How are pituitary adenomas diagnosed?
An imaging test, such as an MRI or CT scan, can show a growth on the pituitary. Apart from radiological tests,lab tests might be done to check the hormone levels in patient’s blood. These tests can confirm the diagnosis of a pituitary adenoma. If patient is having problems with eye sight, the doctor might also ask to take a visual field test to check eye function.
Who treats pituitary tumors?
Pituitary tumors often require care from a team of doctors. Doctors in the team may include:
- Neurosurgeon: a doctor who uses surgery to treat brain and pituitary tumors
- Endocrinologist: a doctor who treats diseases in glands that make hormones
- Radiation oncologist: a doctor who uses radiation to treat cancers and other tumors
- Medical oncologist: a doctor who uses chemotherapy and other medicines to treat cancers and other tumors
How are pituitary adenomas treated?
Pituitary adenomas are usually treated with surgery, medicine, radiation or a combination of these therapies.
Treatment of a pituitary adenoma depends on whether or not it makes excess hormones and, if it does, which hormone it makes. Treatment also depends on whether it's a microadenoma (smaller than 1 centimeter across) or a macroadenoma (1 centimeter across or larger).
Surgery for Pituitary Tumors
Endoscopic pituitary surgery, also called transsphenoidal endoscopic surgery, is the most common surgery used to remove pituitary tumors. Endoscopic pituitary surgery is done with an instrument called an endoscope. An endoscope is a thin, rigid tube that has a microscope, light, and camera built into it.
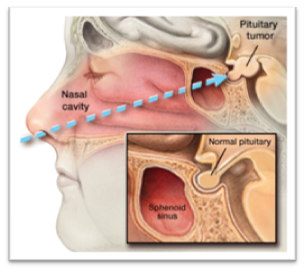
The camera lets your surgeon watch on a television screen while inserting other special instruments through the scope to remove the tumor.

The endonasal approach uses the nostrils as natural surgical corridors to remove pituitary adenomas making it practically stichless ,scarless and cosmetically acceptableas well as effective surgery for pituitary adenomas. Utilizing high-definition endoscopy (surgical telescope), surgical navigation (“GPS for the brain”) and Doppler ultrasound for carotid artery localization, the endonasal approach has evolved into a safe and effective procedure in experienced hands. Major advantages of the endonasal route are: avoidance of brain retraction, minimal or no manipulation of the optic nerves and no facial incisions.
Category:Endoscopic Surgery for Pituitary Adenoma